Cornea Transplantation
What is Cornea Transplantation?
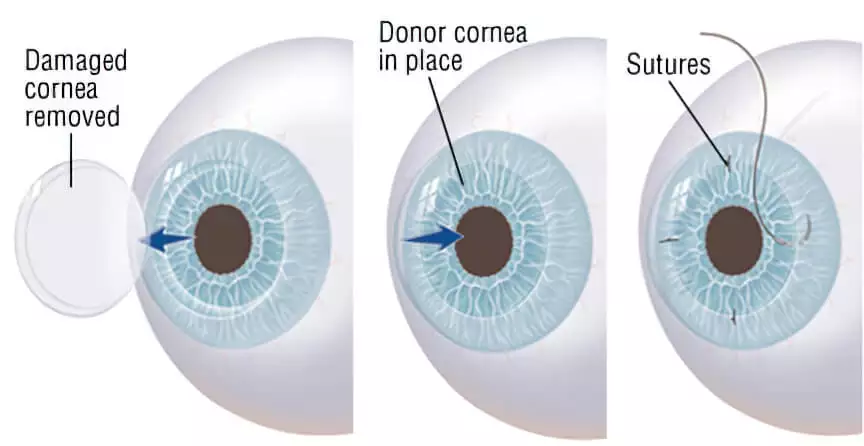
Cornea transplantation, also known as keratoplasty, corneal graft, or eye transplantation, involves the removal of corneal tissue that is deformed or that has lost its transparency, and replacing it with a healthy corneal tissue taken from a deceased donor. Corneal transplant is the most commonly performed and successful transplant surgery with over 40,000 times performed every year.
Why is Cornea Transplantation performed?
Corneal transplantation is performed to treat the following conditions:
- An increase in corneal opacity due to cornea cells being damaged.
- Keratoconus, which is the condition where the cornea takes a conical shape, impeding vision.
- Hereditary corneal diseases.
- Scar tissue or neovascularization that occur as a result of corneal infections, for example herpes simplex virus, HSV.
- Stain formation on the cornea after injury.
Stain formation on the cornea after injury.
What are the conditions for Cornea Transplantation?
To fully benefit from a cornea transplant, the structure of the patient’s eye must be healthy aside from the cornea. If there’s any damage to the patient’s retina there will not be any benefits from the cornea transplant. Specifically, whether a patient will benefit from a cornea transplant will be determined by an ophthalmologist after an ophthalmologic ultrasonography is performed.
Turkey has 2 main “eye banks” with one being in Istanbul and the other being in Ankara. The eye banks are responsible for storing donated corneas, determining whether the tissue is suitable for transplantation and delivering it to the centers where cornea transplantation will be performed. Corneas are taken from recently deceased organ donors who have healthy cornea tissues. It is made sure that the corneas are healthy and do not transmit any diseases. The cornea is a nonvascular tissue, so blood type compatibility is not required.
What are the things to be considered before Cornea Transplantation?
Before the surgery, the patient undergoes a thorough eye examination to ensure that the procedure will be both safe and effective. The patient is asked to get their eye measured before arriving in Turkey to find a matching donor cornea of a similar size. Additionally the patient might need to stop taking certain medication, the medical history of the patient is reviewed by the attending ophthalmologist. The patient should arrive in Turkey a day before the surgery.
How is Cornea Transplantation performed?
Before the surgery begins general or, usually, local anesthesia is administered. Local anesthesia is applied to the eyes and the surrounding areas. Then the eyelids are cleaned thoroughly to minimize the risk of an infection. A small instrument is attached between the eyelids to keep them open during the surgery. The surgeon determines the corneal diameter to be used for corneal transplantation and carefully removes the damaged parts of the cornea through an incision made with a special instrument.If cataract surgery is planned to be done concurrently, the cataract is removed at this point and an intraocular lens is placed in place of the eye’s natural lens. Afterwards, the transparent donor cornea is placed on the recipient bed and sutured using microsurgical methods. At the end of the operation, antibiotic ointment is applied to the eye and the eye is closed with a protective cover.
The surgery takes 30 min to an hour and is done one eye at a time.
What are the things to be considered after Cornea Transplantation?
After the surgery the patient is recommended to:
- Use their prescription medicine as instructed by their ophthalmologist.
- Not put any physical pressure on their eyes and not to rub them.
- Wash their hair with their head tilted, similar to how it's done at a hairdresser, so as to not get any water or soap into the eyes.
- Wear sunglasses while outdoors.
- Avoid strenuous exercises such as swimming, lifting or cycling.
The attending ophthalmologist will decide when the stitches will be removed after the surgery. Usually the stitches are removed a few months after the surgery.
What are the risks of Cornea Transplantation?
Cornea transplantation has an average rejection rate of 5%, this low rate is caused by the cornea usually not having blood vessels and the lack of blood circulation making an immune system response less likely. Risks of corneal transplantation include but are not limited to:
- Infection
- Bleeding
- Excess eye pressure, glaucoma
- Separation of the inner layers of the eye, retinal detachment
- Rejection of the newly transplanted cornea
A corneal transplant can be repeated if necessary without significant drawbacks. Postoperative corneal irregularity may slow the recovery of vision. However, vision will gradually improve within a year after the surgery.
